This guide deals with the question: How do I help my sick child? - The baby's teething problems after birth.
"Doctor, please come quickly, my child is sick. I am very worried and don't know what to do?" Every pediatrician receives these and similar calls almost every day, and he tries to relieve the mother of her worries as soon as possible. Often, however, it takes some time before the doctor can come or the mother and child are with him - hours that become an eternity for any worried mother.Babies' childhood illnesses should be treated

Usually the concern is justified. Sometimes, however, too much fear could be avoided if the mother had some knowledge of childhood diseases. She would then know when immediate medical help is needed and, on the other hand, would not run the risk of dragging on her child's illness, as unfortunately happens again and again. An informed mother will also be able to tell the examining doctor the history of the disease with the necessary calm and objectivity, which makes it much easier to identify the cause.
This article therefore wants to begin to instruct parents and educators about the most common childhood illnesses and the basic care measures. Of course, this should by no means replace a medical consultation or even induce quackery. It is only intended to be a guide for first helping measures that can be initiated by the mother before the medical examination and facilitate home care as directed by the doctor.
First of all, we will talk about the diseases of babies, newborn children and toddlers. It would be wrong to assume that such a small child could not get sick.
A newborn child - it is referred to as such until the umbilical cord has fallen off after 10 to 14 days - experience has shown that although experience has shown that there is hardly any infectious disease, there are very specific disorders during this time that differ fundamentally from those in the later infant due to the age-related physical condition - distinguish between childhood and childhood. In the first days of life in particular, injuries and internal bleeding caused by the birth process, congenital malformations of the heart or the digestive organs can cause serious disorders.
They require immediate treatment by the doctor, which is generally guaranteed as more than 90 percent of all deliveries in Germany take place in clinics or maternity homes.
But what happens later when the young mother has left the hospital and takes care of her child herself? Despite careful care, she will one day discover changes in her child, such as small pimples or spots on the skin that do not seem normal to her. Is that why she should see the pediatrician right away? This is by no means necessary immediately in all cases, as there are a number of changes which can be described as normal in the newborn child and which subside by themselves.
Jaundice in Babies, Children & Infants
The first to be mentioned here is jaundice in babies. It is manifested by yellowing of the skin, mucous membranes and the whites of the eyes and is caused by the presence of large numbers of red blood cells immediately after birth, which were necessary during development in the womb to carry oxygen from the mother to the child .
Since the child is now breathing independently, it no longer needs these superfluous "transport workers". They are destroyed and the blood pigment (hemoglobin) released in the process is converted into bile pigment (bilirubin). As a result, it eventually accumulates in the blood in such an amount that it usually turns yellow on the second or third day of life. So one cannot speak of an illness in the strict sense, although the children are more sleepy and drink less well during this time.
The yellow color usually disappears after one to two weeks. If it lasts longer, there is no cause for concern either, provided the child is thriving normally. However, if this is not the case and a fever occurs, there is a serious cause, e.g. congenital narrowing of the liver. Immediate medical advice is then required.
Breast swelling & inflammation in the baby
Another physiological peculiarity in babies or toddlers is the swelling of the mammary glands, on which a few drops of a milky liquid are secreted when pressed. It is caused by the transfer of maternal hormones to the child during pregnancy or with breast milk and occurs on the fourth to seventh day after birth.
No special treatment is required, as the swelling will subside over the course of two to three weeks. In no case should you try to empty the swollen breasts, as this can cause additional inflammation. So that the laundry does not rub, it is best to put some cotton wool on it.
In addition to the swelling of the mammary glands, an inflammation of the breast known as mastitis can also occur in the baby. It is characterized by reddening, swelling and tenderness and is always associated with fever. This can lead to suppuration and the formation of a mammary gland abscess, which is why medical help is necessary.
Before doing this, the mother should give the child relief from pain with cool, moist compresses. These compresses are best done with an alcohol-water mixture, consisting of one third alcohol (Optal) and two thirds of boiled, cooled water. Boiled chamomile or boron water solution are also suitable.
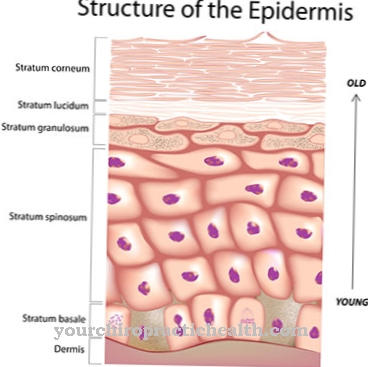
Skin changes & skin diseases in babies
Changes in the skin can also be observed relatively often in the baby's first days, some of which are inflammatory and sometimes non-inflammatory. The non-inflammatory processes also belong, as a rule, to the physiological processes and need not give cause for alarm.
A strong reddening of the skin (erythema neonatorum) is usually observed in babies on the first day of life. In the following days and weeks a rather severe lamellar desquamation (desquamatio neonatorum) sometimes occurs. Small sebum gland vesicles, so-called milia, are also often noticeable. The small yellowish-white dots dot the tip of the nose and sometimes the whole face, but usually disappear again in the course of the first week.
On the other hand, the acne persists for a long time, sometimes up to a few weeks. It manifests itself in blackheads (comedones) standing up against you, which, like breast swelling, are caused by hormonal maternal influences and regress by themselves.
In contrast, in poorly cared for and malnourished infants or babies whose natural resistance is reduced, purulent skin diseases develop easily. The colonization of monobacteria on the skin and in the sweat glands causes either superficial pyoderma or deeper abscesses to form.
Pemphigoid blisters are also characteristic of babies. These lentil- to penny-sized vesicles form easily between the ages of three and eight and usually burst. They are also caused by pus bacteria and tend to be located on the lower abdomen.
In addition to the easy transferability to other toddlers and babies, there is, as with all purulent skin diseases of the newborn, the great danger that pus bacteria migrate from the skin focus via the bloodstream to other organs, where pus foci then develop again. However, the occurrence of such blood poisoning (sepsis) can be avoided if the mother immediately consults a doctor as soon as she discovers any purulent skin changes on her child. It is therefore necessary to carefully examine the entire child's body every day.
Medicines that destroy the pus bacteria, so-called antibiotics, and additional baths with over-manganese acid potassium can in most cases bring about a surprisingly quick healing of all the purulent skin diseases mentioned. The prerequisite for this, however, is that the antibiotics are administered conscientiously and regularly as directed by the doctor. If this is done by mouth, it should be noted that the medication must not be dissolved in the entire bottle formula.
Often times they taste bitter and the child then refuses to eat. In addition, some of the active substances often stick to the bottle wall. Therefore, it is best to dissolve bad-tasting substances in tea sweetened with a sweetener and give them to the child with a spoon, pushing this as far into the mouth as possible under light pressure on the back of the tongue and only taking it out again after swallowing. Then you can drink sweetened tea or breast milk.
Potash baths are best carried out as follows: Do not add the crystals of potassium permanganate, which has an anti-bacterial effect, directly to the bath water, but prepare a concentrated solution beforehand, about one teaspoon of crystals per 100 cubic centimeters of water. It is then added to the bath until the water takes on a wine-red color. It is advisable to use an old, clean cloth to dry it, as the potassium permanganate leaves brown stains. The brown color of the tub can be easily removed with hydrogen peroxide solution and vinegar.
Diseases of the umbilical cord and navel in babies
The navel is also of particular importance in babies. This is where the most vulnerable part of the small child is at this time, and various disorders can arise after the remains of the umbilical cord fall off. Oozing of the navel is particularly common.
At the same time, on closer inspection, after the umbilical folds have been pulled apart, it is not uncommon to find a small red swelling consisting of "wild flesh". It is an increased formation of granulation tissue, which is why this change is also called umbilical granuloma. This excess tissue can be removed in a short time by daily etching with a hellstone pen.
It should be noted, however, that the moistened pencil may only touch the growth and not the intact skin folds, as otherwise etching points will form there. To prevent this, it is advisable to cover the area around the navel well with zinc ointment beforehand. Bathing is allowed despite the granuloma.
If pus bacteria settle in the bottom of the umbilicus, an umbilical ulcer can develop, which is usually covered with a purulent, greasy surface. The umbilical ring and the whole surrounding area are often involved in the inflammation and are very red and swollen. The general condition of the baby is also more or less disturbed. The child no longer drinks properly, vomits intermittently and, as a result, loses weight.
Usually there is also a fever. Since such an inflammation of the umbilical cord can develop into peritonitis or even general blood poisoning (sepsis), the child's life is seriously threatened and the advice of a doctor must be sought. However, these inflammations are not always immediately visible, but sometimes remain covered by the umbilical folds.
It is therefore imperative to examine the bottom of the umbilical precisely every day after the remnants of the umbilical cord fall off. With the help of modern medicine, serious complications can usually be averted if the umbilical cord diseases are recognized in good time.
In this context, a few words should be said about how to prevent navel infections. The remnants of the umbilical cord must be treated in such a way that it promotes rapid drying. It should not be softened by moisture, which is why bathing must be avoided during this time. Drying powder, ideally with the addition of sulfonamides or antibiotics, supports the drying process and prevents colonization with bacteria as far as possible.
Embarrassing cleanliness is the top priority, especially when caring for the umbilical wound, which remains after the umbilical cord has fallen off. The umbilical bandage must consist of sterile, dry bandage material and may only be put on with well washed hands. Once the umbilical wound has healed, the umbilical bandage is removed and the child can be bathed daily.
A number of non-inflammatory disorders can also take place in the navel. The umbilical hernia is the most common. It arises as a result of a congenital enlargement of the umbilical ring and manifests itself as a protrusion on the navel, which becomes clearer when the baby screams and presses, as the contents of the abdomen are pushed forward into the fracture. However, entrapment is extremely rare.
The umbilical hernia does not need to be treated surgically in every case, as is often assumed. Plaster bandages are usually sufficient to regress the break. Only when this is not yet visible at the end of the first year of life must surgical removal be considered in the baby.A child with an umbilical hernia can be bathed despite the plaster bandage, which must be replaced every two weeks.








.jpg)