Myeloproliferative Diseases are malignant diseases of the blood-forming system. The control system of diseases consists in the monoclonal proliferation of one or more hematopoietic cell lines. The therapy depends on the illness in each individual case and can include blood transfusions, blood washing, medication and bone marrow transplants.
What are myeloproliferative diseases?

© blueringmedia - stock.adobe.com
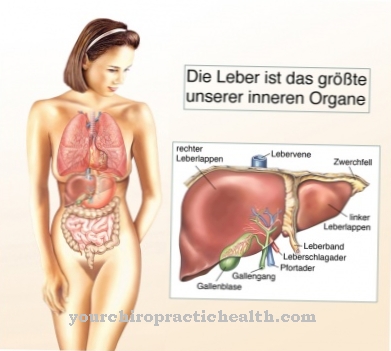
One of the most important blood-forming organs is the medulla ossium, i.e. the bone marrow. Together with the liver and spleen, it forms the human blood system. Different diseases can affect the blood-forming system. The collective term of malignant haematological diseases corresponds, for example, to a heterogeneous group of diseases with a malignant nature that affects the blood-forming system.
The malignant haematological diseases include the subgroup of myeloproliferative diseases. This group of diseases is characterized by a monoclonal proliferation of stem cells in the bone marrow. In the literature, the corresponding diseases are sometimes referred to as myeloproliferative neoplasms.
The American hematologist Dameshek initially proposed the term myeloproliferative syndromes for malignant diseases of the blood system, including diseases such as chronic myeloid leukemia. In the meantime, the disease group of myeloproliferative diseases has established itself, which is based on a malignant degeneration of blood-forming cells of the myeloid series. The group includes more than ten diseases, including polycythemia vera.
causes
The causes of a myeloproliferative disease have not yet been conclusively clarified. According to speculation, risk factors such as ionizing radiation or chemical noxae cause diseases of the blood-forming system. In this context, scientists include benzene and alkylating agents among the chemical noxae.
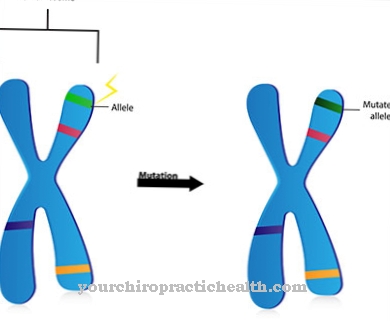
Although it has been proven that the named noxae could all cause corresponding phenomena, in most cases of myeloproliferative diseases a connection with the noxae cannot be directly identified. Researchers have now at least agreed on the suspicion that previously unknown noxae cause mutations in the genome.
These mutations should correspond to chromosome aberrations, i.e. anomalies in the genetically chromosomal hereditary material. The anomalies are currently believed to be the primary cause of disease by researchers. The hypothesis is supported by previously documented case reports of myeloproliferative diseases. In many cases of polycythemia vera there is a mutation in the Janus kinase 2 gene JAK2.
Symptoms, ailments and signs
The symptoms of myeloproliferative diseases can vary in severity and depend on the exact disease in the individual case. However, most of the group's diseases have some complaints in common. In addition to leukocytosis, erythrocytosis or thrombocytosis, for example, can occur.
This means that there is an oversupply of certain blood cells. Especially in the early stages of myeloproliferative diseases, the three mentioned phenomena can occur simultaneously. In addition, patients often suffer from basophilia. An equally common symptom is splenomegaly. In many cases there is also fibrosis of the bone marrow, which is a symptom that is particularly characteristic of osteomyelosclerosis.
Apart from fibrosis, this clinical picture is also associated with extramedullary blood formation. In extreme cases there is a transition to a life-threatening blast surge, primarily in diseases such as CML. Depending on the disease, many other symptoms can occur in individual cases. The presence of all symptoms mentioned here is not absolutely necessary for the diagnosis of a myeloproliferative disease.
Diagnosis and course of disease
Diagnosing myeloproliferative disease is often difficult, especially in the early stages. A clear assignment of the symptoms is usually not possible in the initial stages. In some cases, individual illnesses from the disease group also overlap with one another and make the assignment even more difficult.
For example, polycythemia vera often occurs with or progresses with osteomyelosclerosis. The course of the disease is chronic and is subject to a certain degree of progression. This means that the severity of the disease increases over time and the prognosis is accordingly rather unfavorable.
When should you go to the doctor?
Disorders of the blood flow or irregularities in the heart rhythm must be presented to a doctor. If there is restriction in movement or swelling in the upper body, there is cause for concern. General malfunctions, inconsistencies in digestion or an inner restlessness are signs of an existing illness. A doctor's visit is necessary as soon as the symptoms persist for a long period of time or increase in intensity. If the person concerned complains of a feeling of illness, malaise or sleep disorders, he should consult a doctor. Sudden outbreaks of sweat or a strong nightly sweat production despite optimal sleeping conditions should be presented to a doctor.
An internal cold or heat development as well as an increased body temperature are indications of the organism for an existing health irregularity. Headaches, disturbances in concentration or a decrease in performance must be clarified by a doctor. Changes in the muscular system, an unusual reaction in the body when it comes into contact with preparations containing bases, and a decrease in body weight must be examined by a doctor. A doctor should be consulted if sporting activities or everyday processes can no longer be carried out. Persistent internal weakness, general malaise or emotional problems must be discussed with a doctor. Often a serious illness is hidden behind the complaint that requires immediate action. A doctor should be visited so that a diagnosis can be made.
Treatment and therapy
The therapy of a myeloproliferative disease is symptomatic and depends on the disease in the individual case. A causal treatment is currently not available for the patients. This means that the cause of the disease cannot be resolved. So far, science has not even agreed on the cause.
Until the origin of the disease is not clearly clarified, no causal therapy options will be available. In diseases such as CML, the focus of symptomatic therapy is on conservative drug treatment approaches. The tyrosine kinase activity of the patient should be inhibited.
For example, the affected person is given the tyrosine kinase inhibitor imatinib. Patients with chronic myeloid leukemia also often receive drug therapy with hydroxycarbamide to normalize the white blood cell count. Various measures are used to treat PV.
Bloodletting and apheresis reduce erythrocytes and other cellular blood components. At the same time, platelet aggregation is inhibited to prevent thrombosis. Oral platelet aggregation inhibitors such as acetylsalicylic acid are the drug of choice. Chemotherapy is only indicated if the high number of leukocytes or platelets causes thrombosis or embolism.
If the patient has hypereosinophilia syndrome, imatinib is the treatment of choice. Oral anticoagulation is recommended to prevent embolism. Patients with OMF are observed by haematologists and usually treated using three approaches. In addition to bone marrow transplants, drugs such as androgens, hydroxyurea, erythropoietin or ruxolitinib are available in this context. The third component of therapy is regular blood transfusions.
Outlook & forecast
Myeloproliferative disease has an unfavorable prognosis. It is a malignant disease that is difficult to treat. Without comprehensive medical care, the future prospects worsen considerably. The general life expectancy is reduced for the person concerned. The earlier a diagnosis is made, the sooner therapy can be started. This increases the likelihood of a positive development in the further course of the disease.
Nevertheless, the challenge in treatment lies in coping with the generally progressive development of the disease. Since the cause of the disorder has not yet been fully clarified, doctors decide on the next treatment steps based on the individual situation. The illness represents a strong psychological and emotional burden for the person concerned. In many cases the overall circumstances lead to the development of psychological secondary illnesses.
The patient's body is often so weakened that the therapeutic approaches used do not produce the desired success. Although many complaints are alleviated, it is still difficult to predict how the person's personal development will develop. In addition to drug therapy, regular blood transfusions are necessary to improve general well-being. Overall, the susceptibility to infection increases and with it the risk of further health disorders. For some patients, a bone marrow transplant is the last chance of improvement in overall development.
prevention
Myeloproliferative diseases cannot be prevented with great promise as the causes of the disease development have not yet been conclusively clarified.
Aftercare
Myeloproliferative diseases such as polycythemia vera require extensive follow-up care. Patients with this diagnosis must undergo periodic bloodletting. This lowers the number of blood cells and controls the blood values. If the patient's blood values are well adjusted, he has mastered the first step.
Then you have to think long-term. It is important to maintain the success of the therapy. In addition, aftercare includes making life with the disease as positive as possible. In both cases, patients should be in regular contact with their doctor.
With myeloproliferative diseases, regular follow-up and follow-up checks are extremely important. Examination appointments serve to check the success of the therapy. On the basis of physical well-being, the doctor optimizes the therapy and adapts it to individual needs.
If patients feel uncomfortable between appointments, they should contact their healthcare professional immediately. It is not advisable to wait until the next appointment. Those affected do not have to accept any complaints. The doctor can remedy this with simple means.
In addition, he will review the respective complaints and initiate additional investigations accordingly. There are also other aspects to consider that go beyond the physical limitations. A visit to a psychologist may be beneficial if the illness also affects the patient's psyche.
You can do that yourself
Since myeloproliferative disease is a genetic disorder, the possibilities for self-help are limited. Treatment can be symptomatic. Nevertheless, besides medical treatment, individual measures to improve quality of life can and should be found.
The focus here is on slowing down a negative course of the disease and maintaining the patient's independence.Various methods can be used to achieve this, from which the most appropriate approach for the sick person is chosen. Alternative therapies such as meditation, yoga or other physical exercises can support pain therapy and reduce stress caused by illness. Doctors, psychotherapists or occupational therapists can provide instructions for exercises that can be performed independently at home. Continuous repetition is important for the success of such methods. This is the only way to maintain performance.
Since the courses of the disease are very different, it can help to try different such measures. In general, it is advisable to keep the patient's psychosocial environment in mind. An intact social network provides support and can help deal with the effects of myeloproliferative disease.



.jpg)




.jpg)





.jpg)